Prevalence of MRI lesions in men responding to GP invitations for prostate health screening: a prospective cohort study.
Objective
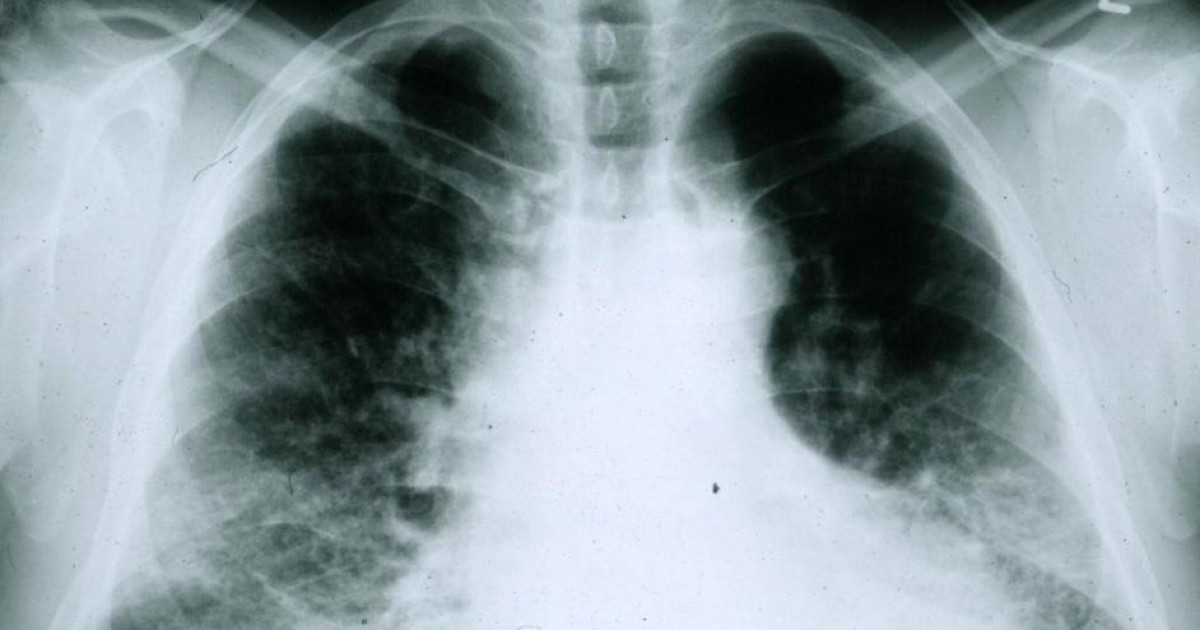
In men with elevated prostate specific antigen (PSA), MRI improves detection of clinically significant cancer and reduces overdiagnosis, with fewer biopsies. MRI as a screening tool has not been evaluated independently of PSA in formal screening studies. We present a community-based systematic assessment of the prevalence of prostate MRI lesions in a population by age.
Methods and analysis
Men aged 50 to 75 years were identified from general medical practice (GP) and randomly selected to invite them for MRI and PSA examinations. Man undergoing MRI positive or increased PSA density (≥0.12 ng/mL 2 ) is recommended for the National Health Service (NHS) standard assessment of prostate cancer.
Results
Eight GP practices sent invitations to 2,096 men. 457 men (22%) responded and 303 completed both examinations. Older white men were more likely to respond to the invitation, and black men had a 20% acceptance rate than white men.
One in six men (48/303 men, 16%) had an MRI scan positive, and 1 in 20 men (16/303.5%) had only increased PSA density. Following the NHS assessment, 29 men (9.6%) were diagnosed with this disease clinically significant cancer and 3 males (1%) with clinically insignificant cancer.
Two out of three men with MRI positive and more than half of men with clinically significant disease have a PSA<3ng/mL.
|
conclusion
Prostate MRI may have value in screening independent of PSA. These data will enable modeling the use of MRI as a primary screening tool to inform larger prostate cancer screening studies.
|
Comment
The REIMAGINE study, published in BMJ oncology, is the first study to use prostate-specific antigen (PSA) density MRI scans to assess the need for further standard NHS testing. Of the 29 participants with advanced prostate cancer, 15 had a ‘low’ PSA score meaning they were not referred for further testing under the current system.
Currently, men over 50 in the UK can request a PSA test if they have symptoms or are concerned about prostate cancer. Previous screening studies have used a PSA level of 3 ng/mL or higher as a reference point for additional tests to detect prostate cancer, such as a biopsy.
Although previous studies have found that the combination of PSA and/or DRE testing, followed by a biopsy if the disease is suspected, helps reduce mortality from prostate cancer by 20% after 16 years, this approach has also been associated with overdiagnosis and overtreatment. lower risk cancer.
In recent years, the introduction magnetic resonance as a first step in investigating men at high risk of developing prostate cancer has prevented one in four men from having unnecessary biopsies, which are invasive and can lead to complications.
It is hoped that the use of MRI as a screening tool offered to men without their request will further reduce mortality from prostate cancer and over-medication.
For the study, researchers invited men aged 50 to 75 to undergo MRI and PSA tests.
Of the 303 men who completed both tests, 48 (16%) underwent an MRI scan positive which indicates the possibility of cancer, although it only has a median PSA density of 1.2 ng/mL. 32 of these men had PSA levels Lower than the current screening benchmark of 3 ng/ml, which means they will not be referred for further testing using the currently used PSA test.
Following the NHS assessment, 29 men (9.6%) were diagnosed with cancer requiring treatment, 15 of whom had severe cancer and a PSA of less than 3 ng/ml. Three men (1%) were diagnosed low risk cancer which does not require treatment.

“Internet trailblazer. Troublemaker. Passionate alcohol lover. Beer advocate. Zombie ninja.”