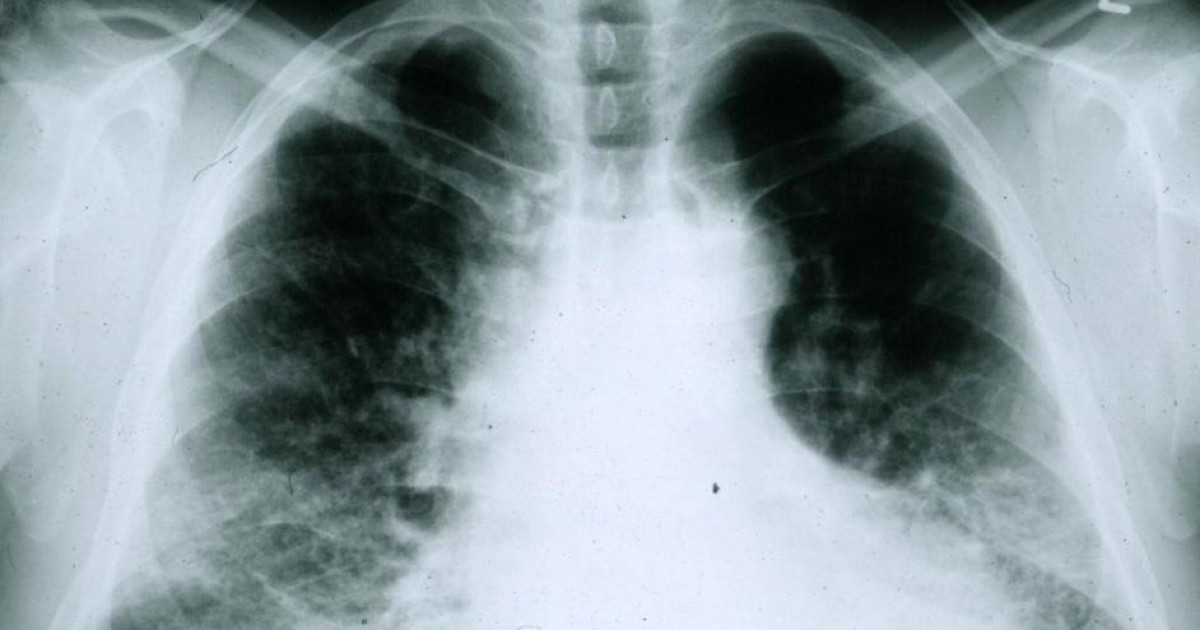
The terrible epidemic generated by the SHARS-Cov-2 virus has exposed the deficiencies of our health system; all countries in the EU have suffered the serious consequences of the virus that has left us; Even the most economically developed countries are unable to manage epidemics effectively. Only a few Nordic countries have experienced lower incidences, both in infection and death numbers. Italy, on the other hand, has been the country where the worst coronavirus has wreaked havoc. Spain has followed closely.
In our country, the start of the epidemic was not managed effectively, underestimating the consequences it could have on us. We see ourselves reflected in the situation that Italy is in; but the Ministry of Health with its “experts”, had no idea how to see what was coming; leading to hospital burnout and emergency primary care, as well as a very high incidence of hospitalization and death.
However, the government has managed vaccinations effectively in coordination with Autonomous Communities and has reached over 80% of the population by the end of 2022; coincided with the OMICRON variant, the most infectious up to that time; after that, the epidemic became a mild respiratory infection in most cases, except in those who were seriously or persistently ill. Management of vaccination schedules is done (and it must be said) better than in most EU countries; although I am very different from other epidemic management that has been done.
Due to all of the above, Spain has experienced a significant decline in terms of the health of its citizens; We have to consider that our country invests in health less than the EU average; which in 2022 amounts to 2,244 euros per resident. Spain in the same year invested 1854 euros, behind France, Germany and Italy. Despite this, our country is in 25th place in the ranking of 192 most important countries: but that is not enough.
It is a priority need for Spain to increase resources in public health; especially in “primary care”, the filters are basic and necessary to avoid system saturation, especially the hospital system. We have corroborated that increased investment in “primary care” results in substantial improvements in the health of citizens; especially the elderly, who are most vulnerable to suffering from the five most common diseases.
Another very important thing to consider is the waiting list. Countries like France, Germany, Norway and Finland have shorter waiting lists than ours; both in surgery and in other treatments; Let’s give a few examples: in Spain in “primary care”, the percentage of patients who have to wait more than one day to be seen by a general practitioner has increased from 55.1% before the epidemic to 78.1% today; Likewise, in the case of specialists, the percentage of patients seen with a delay of more than three months has increased from 25% before the arrival of the coronavirus to 37.8% in the last wave of studies. In surgery, the wait for intervention has increased tremendously, largely due to the epidemic; reached 148 days in the last year: the Community of Madrid has a much shorter waiting list than the national average, with 64 days to access surgical intervention; less than half the national average.
However, regarding Primary Services, the Community of Madrid lacks sufficient resources to offer quality medical services. Since May last year, the Community of Madrid has been experiencing a strike by “primary care” doctors and, to a lesser extent, hospitals; Fortunately, the Ministry of Health has reached an agreement with doctors and unions; increasing medical costs to 450 euros per month for family doctors and pediatricians; and 500 euros for those who choose the afternoon shift. It is also limited to 20 patients per day for family doctors and 30 for pediatricians. Regarding the hospital strike, the unions have reached an interim agreement with the Ministry; cancel the strike they had planned a few days ago; and they expect some important actions to be completed in the coming days, perhaps after Easter.
If we want to significantly improve Primary Care in Autonomous Communities, the following points must be considered
First: limiting the number of patients per doctor, both in family doctors and in paediatricians (Agreement reached in the Community of Madrid)
Second: increased costs of doctors and nursing staff (also resolved in Madrid) Third: promoting clinical sessions between doctors from outpatient clinics and from hospitals; important for ongoing training of the former, which will improve the quality of care.
A Fourth point What should be considered is to increase the recruitment of doctors with training in family medicine. All of this requires significant resources directed at health centres. The welfare state is mainly based on Health, Education and pensions; but in my opinion, Health is perhaps the one that, given the immediacy of the services requested, needs more attention.
We have to consider that there are five pathologies that occur most often, and they account for more than 80% of the diseases of the population. These are the following: diabetes, hypertension, COPD, rheumatic diseases and finally, heart failure. This pathology should be treated by a “primary care” doctor first, before referring the patient to a specialist. Therefore, as I mentioned earlier, it is very important to provide the “health center” service with the necessary human resources to treat patients adequately.
Investments in technology are not as important as in primary health care; Hospitals in Spain are endowed just as in Europe with the best high-tech equipment; This is not a public health problem in Spain, but there is a serious shortage of “health center” services.
Finally, I will make a brief reference to service outsourcing: I believe that it is an important complement to public health; But provided it is done wisely. Outsourcing carried out in the UK since 2012 has not yielded the expected results; on the contrary: medical care for citizens is getting worse (1). I support rational outsourcing, just as I support shared services.
But always do it with hospitals and referral and excellence centers. This complements public health and shortens waiting times; both in consultation and in complementary tests. In Spain, especially with this government, there is no good concept of outsourcing, it is believed that all services should be provided through public health; and that’s not entirely true.
After surviving the worst known epidemic since 1918, it was important to increase investment, especially in health centres. The welfare state cannot be consolidated if we don’t. It goes without saying that there is no position between them to make a decision; As only an economist with knowledge of health management, I limit myself to giving my impressions: whatever the value.
(1): Aaron Reeves, Professor, Oxford: The Lancet.

“Internet trailblazer. Troublemaker. Passionate alcohol lover. Beer advocate. Zombie ninja.”